Acute Kidney Injury (AKI)
Written by Kacey Klemesrud, 3rd year Veterinary Student • 2018 Scholar
History

Gigi is a two-year old, spayed female Toy Poodle. She presented with a two-day history of anorexia, lethargy, loose stools, and vomiting.
Physical Exam
The following abnormalities were noted:
- Retained deciduous upper canine teeth
- More common in small dog breeds, like toy poodles1
- Incidental finding in this case
- Moderate periodontal disease- incidental finding in this case
No significant findings were present on physical examination. Abdominal palpation, cardiac auscultation, lung sounds, hydration level, temperature, etc. were all within normal limits. Further diagnostics (bloodwork, urinalysis, radiographs, ultrasound) were essential in treating Gigi’s illness.
Diagnostics
Bloodwork- Complete Blood Cell Count (CBC) and Chemistry
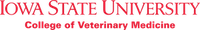
The major diagnostic findings in Gigi’s blood chemistry profile involve the large increases in blood urea nitrogen (BUN) and creatinine. The condition in which an animal has an increase in BUN and creatinine is called azotemia. There are three general pathophysiologic mechanisms that may cause azotemia (see Figure 1):
- Pre-renal azotemia: dehydration or low blood pressure leads to lack of blood flow through the kidney and decreased clearance of BUN and creatinine. Gigi appeared to be well hydrated on physical exam, so the azotemia is unlikely caused by a pre-renal issue.
- Post-renal azotemia: ruptured bladder, or obstruction leads to decreased clearance of BUN and creatinine from the body. Gigi was still able to urinate, so an obstruction or ruptured bladder is an unlikely cause of the azotemia.
- Renal azotemia: Injury or disease of the kidney leads to decreased kidney function and clearance of BUN and creatinine. Loss of kidney function is the most likely cause of Gigi’s azotemia due to other diagnostic outcomes, such as those seen below, and the lack of evidence for pre-renal and post-renal abnormalities.1,2
The kidneys are the main route of excretion for phosphorus in the body. Thus, with Gigi’s loss of renal function, phosphorus was unable to be excreted.2
Symmetric Dimethylarginine (SDMA) is a more sensitive diagnostic indicator of loss of renal function. It detects renal disease when there is as little as 40% loss of renal function, whereas BUN and creatinine can only be detected with greater than 70% loss of renal function.3
Apart from changes in kidney function, the bloodwork also revealed the following abnormalities.
Alkaline Phosphatase (ALP) is an inducible liver emzyme that is released in the case of cholestatasis (decreased bile flow).4 Abdominal ultrasound also showed signs of cholangitis, which supports the evidence of cholestasis.
Thrombocytopenia (low platelet count) can be caused by several factors, including infections, immune-mediated damage, excessive clotting, drugs, toxins, etc.1
Urinalysis
Because the bloodwork results indicated a change in kidney function, a urinalysis was performed via cystocentesis.
The specific gravity of urine (USG) helps determine if the kidneys can actively concentrate or delute urine. In the face of azotemia, we would expect the to be concentrated with USG > 1.030, but Gig's USG was 1.016, indicating the kidneys are not functioning properly.5
Cocci bacteria were present in the urine, which could be causing a urinary tract infection that ascended to the kidneys or could be an incidental finding.
Infectious Agent Tests
4DX Test- The 4DX test recognizes ehrlichia, anaplasmosis, heartworm, and lyme disease.
- Lyme disease is one of the most commonly transmitted tick-borne diseases. Although it usually causes arthritis-like changes, it can also rarely cause acute renal injury as well.1 However, Gigi’s test came back negative for lyme disease.
- Ehrlichia is another tick-borne disease that often causes thrombocytopenia.1 Due to Gigi’s pronounced thrombocytopenia and prolonged clotting times, ehrlichia is an important differential to consider. However, Gigi’s test was negative for ehrlichia.
Leptospirosis Antibody Titer and PCR
- One commonly missed cause of acute renal injury and hepatopathy is leptospirosis. This pathogen can have severe effects on multiple systems, including renal and hepatic insults. In addition, leptospirosis is zoonotic (affecting people), thus careful precautions must be taken when handling the animal, especially it's urine.1 Gigi was nagiative for leptospirosis and PCR and antibody titers.
Ultrasound
- Mild bilateral chronic renal disease- in Gigi’s case, these chronic changes could have developed due to the acute kidney injury. However, she could have also been more at risk for acute renal injury with a pre-existing chronic kidney disorder. Regardless, Gigi’s kidney values should continue to be monitored closely.
- Cholangitis- biliary sludge or cellular debris. This is consistent with her increases in ALP.
Diagnosis
The diagnostic changes indicated that Gigi was battling three major conditions: acute renal injury, thrombocytopenia, and a hepatopathy. Lyme disease, ehrlichia, and leptospirosis were ruled out of the list of differential diagnoses. Because the cocci were seen in the urine, it is possible that the bacteria ascended to the kidney’s, causing a renal injury. However, the definitive cause of Gigi’s illness is unknown. Figure 1 below shows the diagnostic process and other possible differentials for this case.
Figure 1- Diagnostic flowchart for Gigi’s acute renal injury, thrombocytopenia, and hepatopathy1,2,4
Prognosis
Prognosis for Gigi was grave. With her severe multisystemic disease and worsening kidney values, she required intensive care and critical surveillance. Typically, death or euthanasia is expected in half of the acute renal injury cases. In addition, half of those that survive will develop chronic kidney disease.2 Gigi’s owner was notified of these concerns and elected to pursue aggressive treatment of Gigi’s disease.
Treatment & Monitoring
Fluid Therapy, Normosol-R (18 ml/hr)
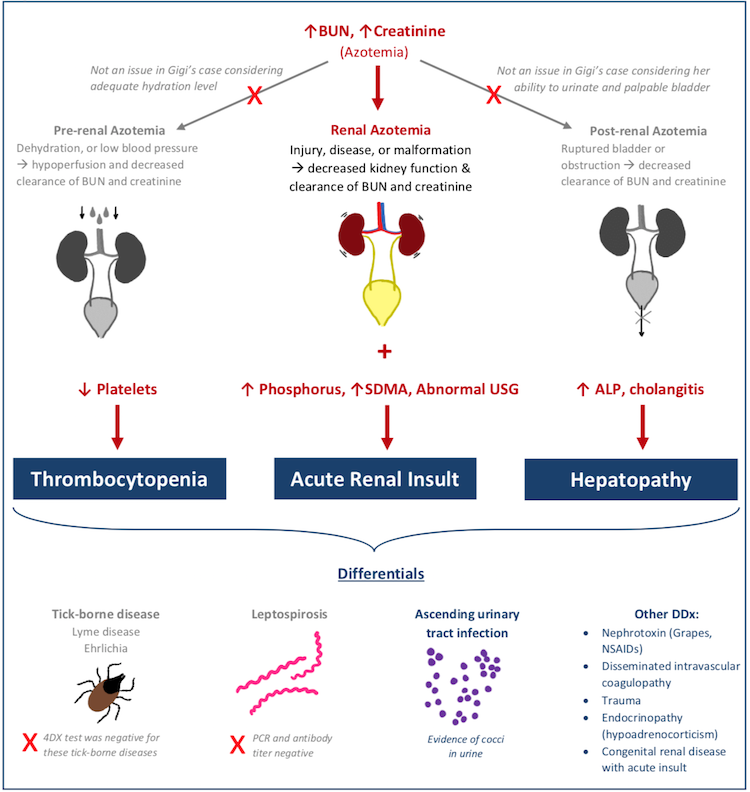
Fluid therapy is one of the most important treatments to provide to renal failure patients. Because the kidney’s play a large role in fluid regulation in the body and excretion of metabolic wastes, fluid administration is given to AKI patients in attempt to increase glomerular filtration rate and encourage normal filtration. The goal is to maximize the amount of fluids administered to the animal without overexerting the kidneys and causing fluid buildup. However, in many cases like Gigi, the animal becomes oliguric, or is unable to produce larger, normal volumes of urine.4
Fluid Therapy, Normosol-R (18 ml/hr)
Fluid therapy is one of the most important treatments to provide to renal failure patients. Because the kidney’s play a large role in fluid regulation in the body and excretion of metabolic wastes, fluid administration is given to AKI patients in attempt to increase glomerular filtration rate and encourage normal filtration. The goal is to maximize the amount of fluids administered to the animal without overexerting the kidneys and causing fluid buildup. However, in many cases like Gigi, the animal becomes oliguric, or is unable to produce larger, normal volumes of urine.4
Initially, Gigi was started on a fluid rate of 18 ml/hr, which is about three times the level of maintenance fluid levels, to correct for slight dehydration. Once hydrated, it was expected that Gigi’s urination levels would increase rapidly to 2-5 ml/kg/hr (6-15 ml/hr for Gigi).4 However, the technicians that monitored Gigi each hour noticed she was producing little to no urine at all. Because Gigi was at risk for fluid overload, a urinary catheter was placed to monitor her urinary output and adjust fluid administration accordingly. As shown in the Figure 2 below, at 4 hours post U-cath placement, Gigi’s urinary output was exceedingly low, especially in regards to the volume of fluids being administered. Thus she was started on furosemide, a diuretic, to help increase urine output. When Gigi reached a high urinary output of about 90ml/hr and her azotemia was improving, the furosemide CRI was discontinued and fluid rates were decreased. Once she was able to maintain her urine outputs at a similar rate to her intravenous fluids, her urinary catheter was removed.
Furosemide, Constant Rate Infusion (1.3mg/kg/hr)
Loop diuretic that encourages the excretion of sodium and water to increase urine output.6 This drug gave Gigi’s kidney’s the boost they needed to increase urination levels and decrease her risk of fluid overload.
Treatment & Monitoring
Gigi was hospitalized and monitored for 7 days. During that time the following medications were administered:
Fluid Therapy, Normosol-R (continued)
Another important aspect of Gigi’s fluid therapy treatment is the type of fluid administered. In oliguric patients
like Gigi, it is common for potassium to build up in their bloodstream, as it is not able to be excreted from the body. Another term for increased potassium is hyperkalemia.2 As Gigi was being monitored, her potassium levels were markedly increased. Thus, it was important to administer fluids that do not contain potassium. The fluid that Gigi was given was Normosol-R, which contains sodium and chloride in the same concentrations as what’s in Gigi’s blood naturally.
Enalapril (1.25mg PO, BID)
During Gigi’s struggle with oliguria, fluids built up in her body causing some signs of fluid overload such as increased blood pressure, decreased heartrate, and peritoneal effusion.4 In attempt to decrease Gigi’s blood pressure, Enalapril was scripted. Enalapril is an angiotensin converting enzyme inhibitor and antihypertensive drug that was given initially twice a day by mouth, then tapered off as Gigi’s signs of hypertension improved.6
Amlodipine (1.25mg PO, SID)
Amlodipine is a calcium channel blocker used as another form of antihypertensive medication.6 Although similar to enalapril, the mechanism of action is different. Often times, it necessary to use a combination of different antihypertensive drug classes in order to get the best outcome.7 Thus, both amlodipine and enalapril were included in Gigi’s treatment plan for hypertension.
Buprenorphine (0.05mg, transmucosally, TID)
As Gigi was being monitored, she became painful in her abdomen during palpation. Buprenorphine is an opioid analgesic that has had great success for the treatment of pain in canine patients when administered transmucosally.6
Unasyn-ampicillin & sulbactam- (90mg IV, TID)
Antibiotic that was administered to Gigi upon entry to treat the possible bacterial infections that were on our differential list, leptospirosis or urinary tract infection.6
Amoxicillin-Clavulanate Potassium, CLAVAMOX- (62.5mg PO, BID)
Longer course antibiotic scripted for Gigi due to long-term use of urinary catheter and risk for ascending urinary tract infection.
Pantoprazole (144mg IV)
Because Gigi’s uremic acids were high, she was at risk for gastric ulceration. Pantoprazole is a proton pump inhibitor administered for its gastroprotective properties.6
Famotidine (2.5mg PO, BID)– Histamine type II receptor antagonist also used to help reduce the risk of gastric ulcers6
Maropitant (3mg IV, SID)
Neurokinin-1 receptor antagonist that acts in the emetic center to prevent nausea and vomiting.6
Capromorelin, ENTYCE (7.5mg PO, SID)- ghrelin receptor agonist that is labeled for appetite stimulation in dogs.8
Denamarin (90mg PO, SID)- Hepatoprotectant given to Gigi due to her elevated ALP liver values and cholangitis.6
Recovery and Outcome
During Gigi’s hospitalization, her kidney values remained the main point of concern and bloodwork was repeated daily to monitor BUN and creatinine. Figure 3 shows the trends in Gigi’s kidney values over time. Once these values stabilized she was discharged, but returned for three days to ensure she was able to maintain these on the medications that were sent home.
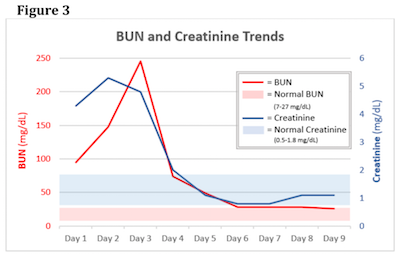
Figure 3
As mentioned previously, BUN and creatinine values increase only when there is more than 75% loss of kidney function. Thus, although the kidney values are improving, there could be underlying damage to Gigi’s kidneys. SDMA was rechecked the day after she was discharged and it remained elevated, indicating that there is chronic damage.3 However, Gigi has remained clinically healthy for each recheck. Her platelet numbers and liver values also normalized with therapy. Gigi’s owner will continue to monitor her for any changes at home, but for now Gigi is back to her normal, sweet, playful self.
References & Citations
- Tilley, L.P., Smith, F.W.K. (2016). Blackwell’s Five-Minute Veterinary Consult: Canine and Feline (6th Ed). Ames, Iowa: Wiley Blackwell.
- Nelson, R.W., Couto, C.G. (2014). Small Animal Internal Medicine (5th Ed). St. Louis, Missouri: Elsevier Inc.
- Bilbrough, G, et al. (2018). IDEXX Catalyst SDMA Test for in-house measurement of SDMA concentration in serum from dogs and cats. IDEXX Laboratories. Retrieved from https://www.idexx.com/en/veterinary/reference-laboratories/sdma/. Online PDF.
- Bonagura, JD, Twedt, DC. (2014). Kirk’s Current Veterinary Therapy (15th Ed.). St. Louis, Missouri: Saunders Elsevier Inc.
- Smets, P.M.Y., Meyer, E., Maddens B.J.E., Ducheteau, L., and Daminet, S. (2010). Urinary Markers in Healthy Young and Aged Dogs and Dogs with Chronic Kidney Disease. Journal of Veterinary Internal Medicine, 24, 65-72. https://doi.org/10.1111/j.1939-1676.2009.0426.x.
- Plumb, D.C. (2011). Plumb’s Veterinary Drug Handbook. (7th Ed.). Wiley-Blackwell.
- Buoncompagni, S., and Bowles, M.H. (2013). Treatment of Systemic Hypertension Associated with
Kidney Disease. Compendium: Continuing education for veterinarians. Online PDF. - Zollers, B., Rhodes, L., and Heinen, E. (2016). Capromorelin oral solution (ENTYCE®) increases food consumption and body weight when administered for 4 consecutive days to healthy adult Beagle dogs in a randomized, masked, placebo controlled study. BMC Veterinary Research, 13(10). https://doi.org/10.1186/s12917-016-0925-z