Sissy's Case summary
Written by Siyu Xiao • 2021 Scholar
Presentation/History
Sissy, an approximately 3.5 years old female spayed Yorkshire Terrier, presented to IVS for dark brown, watery stool. Recently, the owner noticed Sissy did not eat well and was advised by the primary care vet to try chicken and rice. She was fed rotisserie chicken, and then the owner noticed vomitus at home. There were multiple dogs at home, and the owner was unsure if Sissy vomited. Sissy later started to show signs of decreased energy and was brought to IVS for emergency evaluation of her diarrhea and potential vomiting.
Sissy had a history of urinary tract infection (UTI) with development of a single bladder stone and was treated with Clavamox (an antibiotic) for 10 days.
Physical Exam
Sissy’s body condition score was 5/9, and her capillary refill time (CRT) was about 3 seconds. The only significant finding on her physical exam was dark brown stool on rectal exam. There was no pain associated with abdominal palpation on the day of hospitalization. However, signs of abdominal pain developed 24 hours later.
CRT reveals information of patient’s peripheral perfusion status. Normally, CRT should be less than 2 seconds. Sissy had a prolonged CRT, suggesting decreased peripheral perfusion. Dehydration is one of the common reasons for decreased peripheral perfusion.
Diagnostics
Based on her history and presentation, bloodwork (CBC/ Chemistry/cPL) and abdominal radiographs were advised. Owner consented to those diagnostics. By interpretation of bloodwork, veterinarians can grasp a general view of patient’s organ function which is crucial for disease diagnosis. A cPL is a snap test developed by IDEXX specific for canine pancreatitis screening. Radiographs, important diagnostic tools in modern veterinary medicine, can give a general evaluation of patient’s internal organs. At IVS, all images will be sent to a board-certified radiologist for further evaluation. The following were results of Sissy:
CBC:
Mild erythrocytosis (elevated red blood cell count) with elevated hematocrit (HCT)
- Red blood cell (RBC) count and HCT value are commonly used to evaluate if patient experienced any types of anemia, dehydration or other diseases.
- Mildly elevated RBC count and HCT most commonly related to dehydration, especially in patients with a history of vomiting and/or diarrhea.
Slightly decreased mean corpuscular volume (MCV)
- Decreased MCV, commonly seen in patient with iron deficiency anemia or liver disease.
Reticulocytosis (elevated reticulocytes)
- Reticulocytes are immature red blood cells. Reticulocytosis is usually a sign of regeneration/ erythropoiesis (red blood cell generation).
Neutrophilic leukocytosis (increased white blood cell counts due to increased neutrophils)
- Presentation of leukocytosis, especially with neutrophilia suggests some kind of inflammatory response happening within the patient’s system.
Blood smear noted reticulocytosis and leukocytosis which was consistent with the CBC report.
Chemistry:
Hypoglycemia (decreased blood glucose)
- Sissy’s initial blood glucose (BG) showed moderate hypoglycemia which was concerning. Common causes of hypoglycemia are increased consumption (e.g. sepsis, neoplasia, hyperinsulinemia), decreased production (e.g. hepatic insufficiency, starvation, hypoadrenocorticism) or artifacts (e.g. prolonged blood processing).
- Since prolonged hypoglycemia may lead to neurologic signs, such as seizure. IV dextrose was given and BG was rechecked in the next 48 hours. The glucose level went back to normal after the treatment.
Elevated blood urea nitrogen (BUN)
- BUN and Creatinine are analytes used to evaluate kidney function. Elevated BUN and/ or Creatinine is called azotemia. In general, there are three types of azotemia: pre-renal, renal and post-renal. Most common cause of pre-renal azotemia is dehydration, especially when BUN is disproportionally elevated versus creatinine.
- Sissy had elevated BUN, but her creatinine level was at the lower margin of the reference interval (RI). Based on Sissy’s clinical presentation of diarrhea, prolonged CRT, and elevated BUN, dehydration was considered as the main contributor of her azotemia. Kidney function seemed to be less of a concern at this point.
Panhypoproteinemia
- Decreased total protein including both albumin and globulin is termed as panhypoproteinemia.
- Albumin is a main contributor to maintain proper oncotic pressure and synthesized in liver. Decreased albumin (hypoalbuminemia), is commonly caused by decreased production (malnutrition, hepatic insufficiency, inflammation, etc.), increased loss (protein-losing enteropathy / nephropathy, severe hemorrhage, third spacing of fluid, etc.) or excess fluid administration. In Sissy’s case, we were more concern of hepatic insufficiency, inflammation (pancreatitis), and protein-losing enteropathy (PLE).
- Globulin is the second type of proteins. Sissy also had decreased globulin (hypoglobulinemia). Common causes of hypoglobulinemia include PLE, hemorrhage, and decreased of immunoglobulin.
- In summary, based on all other information, we were more concerned with hepatic disease, PLE, inflammation (pancreatitis) and hemorrhage through gastrointestinal tract at the moment.
Hypocalcemia (decreased total calcium)
Sissy had decreased total calcium level. Calcium in blood usually have three forms: free ionized calcium, protein bound calcium and complex calcium. Total calcium level is commonly influenced by various factors, including blood pH, blood protein level, etc. In patients with decreased total protein, decreased total calcium commonly presents as well because of decreased protein-bound calcium. Also, mild hypocalcemia is commonly seen in patient with pancreatitis.
Slightly increased alkaline phosphatase (ALKP)
- ALKP is a non-tissue specific inducible enzyme. The tissue sources of ALKP include hepatocyte, biliary epithelium, osteoblasts and mammary epithelium. Elevation of ALKP in dogs is commonly associated with hepatobiliary disease, corticosteroid, mammary gland tumor or increased osteoblast activity. In this case, mild increase ALKP was most likely related to liver disease or cholestasis secondary to pancreatitis.
Hypocholesterolemia (decreased cholesterol)
- Cholesterol is an important precursor of cholesterol ester, bile acids and steroid hormone. Low-density (LDL) and high-density lipoprotein (HDL) have highest concentration cholesterol. Liver is a main source of cholesterol. Low cholesterol can be due to decrease of LDL, HDL and etc. Common causes of hypocholesterolemia include PLE, hepatic insufficiency, neoplasia, etc.
Significantly increased amylase and lipase
- Level of amylase and lipase are used as indicators of pancreatic injury. Pancreatitis is the most common reason for significantly elevated serum amylase and lipase, especially in dogs with clinical signs of vomiting, diarrhea and inflammation.
cPL snap test:
- Abnormal cPL snap test is usually an indicator of canine pancreatitis.
Elevated fasting bile acid:
- Bile acids are synthesized by hepatocytes from cholesterol and excreted into bile. The function of bile acids is to emulsify fat in intestine and facilitate nutrient absorption. Bile acids are highly conserved via enterohepatic circulation. Bile acids is a one of direct liver function test.
- Due to concern of Sissy’s liver function, the patient was fasted and tested for bile acids. The level of fasting bile acid was severely increased, indicating of liver disease or portosystemic shunt (with normal alanine aminotransferase, ?-glutamyltransferase, less concern of cholestasis).
Radiograph:
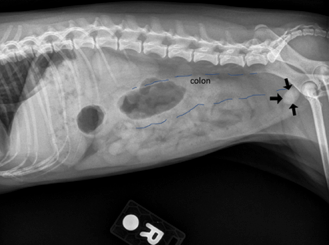
On this right lateral view, there was an ovoid mineral opaque object at the anatomic location of urinary bladder. According to the radiologist, it was a single bladder stone (pointed by black arrows) which was consistent with Sissy’s history. There was reginal poor serosal detail in the cranial abdomen. The colon was filled with gas and soft tissue opaque fluid (outlined by blue dashes) which was consistent with diarrhea history.
Diagnosis
The patient was diagnosed with severe pancreatitis, hepatopathy or portosystemic shunt, and urinary tract infection. Pancreatitis
In summary, the patient presented to ER for bloody, watery diarrhea with a history of urinary tract infection and development of a bladder stone. On physical exam, the patient showed signs of dehydration and bloody, watery stool on rectal exam. For lab work, the following abnormal findings together were consistent with pancreatitis: abnormal cPL snap test, neutrophilic leukocytosis, elevated amylase and lipase, imaging patterns of reginal peritonitis and gastroenteritis.
On chemistry, patient was presented with hypoglycemia, hypocholesterolemia, hypoalbuminemia. Sissy had significantly elevated fasting bile acids level. On CBC, patient had signs of mild microcytic normochromic erythrocytosis with reticulocytosis, which made it hard to completely rule out mild regenerative anemia. Because the patient was severely dehydrated, this might mask mild signs of regenerative anemia. Such pattern of hypoglycemia, hypocholesterolemia, hypoalbuminemia, mild elevated ALKP, signs of mild microcytic regenerative anemia and significantly elevated fasting bile acids was highly suggestive of liver insufficiency or portosystemic shunt. However, considering the patient was a Yorkshire Terrier with history of diarrhea, it was hard to completely rule out PLE. Yorkshire Terrier is a type of breed predisposing to PLE. Further diagnosis was required.
Treatment Plans
After discussion with the owner, Sissy was provided with supportive care for pancreatitis, hepatopathy, hypoglycemia and UTI. Considering her underlying problem, the owner was suggested for a consultation at the internal medicine department for her liver and urinary issues and owner consented.
Medication:
- Intravenous (IV) fluids: Isotonic fluids with 2.5% dextrose added given intravenously. An IV catheter was placed and IV fluid rate was adjusted based on monitoring the patient hydration status. Fluids are important to correct hypovolemia, dehydration and electrolyte/ acid-base imbalance. The 2.5% dextrose was added as a constant rate infusion in order to restore the patient’s blood glucose level. Blood glucose (BG) levels were rechecked every 4 hours for the next 48 hours. The BG returned back and maintained within normal RI after initiation of fluid therapy.
- Maropitant: Maropitant was given IV for nausea control. Maropitant is a neurokinin 1 receptor inhibitor that commonly used as antiemetic.
- Metronidazole: An antibiotic and antiparasitic drug indicated for enteric anaerobic infection. Sissy was treated with metronidazole twice a day IV in order to relieve her symptom of diarrhea.
- Fentanyl CRI: A FCRI was started the second day of her hospitalization for abdominal pain related to pancreatitis and was discontinued before discharge when her clinical signs improved. Fentanyl is a schedule-II controlled opioid analgesic in the United States. In cases of pancreatitis, studies showed that aggressive pain control is crucial for successful management of pancreatitis.
Discharge
Sissy was hospitalized for about 72 hours at IVS with supportive care and continuous monitoring. On day 3 of hospitalization, her physical exam results were unremarkable and patient was stable. Discharge was discussed with owner and owner consented. The emergency veterinarian also recommended an internal medicine consultation as soon as possible to further address Sissy’s liver and urinary issues. Sissy was discharged with metronidazole oral suspension (to give orally every 12 hours) and maropitant (1/2 tab every 24 hours for 4 days). Oral metronidazole aimed to decrease bacterial deamination and reduce the production of aromatic amino acids, short chain fatty acids and false neurotransmitters to prevent hepatic encephalopathy and diarrhea. She was suggested to be fed on small meals every 4-6 hours with limited exercise.
Follow-up
Sissy was transferred to the internal medicine department for consultation the next day of discharge from ER. A urinalysis was performed showed presences of inadequate urine specific gravity and cocci bacteria. Urine culture and gastrointestinal panel were performed with pending results. Abdominal computed tomography (CT) scan confirmed that she had extrahepatic portosystemic liver shunt (blood flow bypasses the liver by direct connection of portal vein to systemic circulation) with peritoneal effusion (fluid accumulation in peritoneal space) and a large cystolith (bladder stone).
References & Citations
- Willard, M. D., & Twedt, D. C. (2004). Gastrointestinal, Pancreatic, and Hepatic Disorders. Small Animal Clinical Diagnosis by Laboratory Methods, 208–246. https://doi.org/10.1016/B0-72-168903-5/50014-8
- https://eclinpath.com/
- https://www.vetfolio.com/learn/article/canine-and-feline-pancreatitis
- https://todaysveterinarypractice.com/diagnosis-treatmenta-case-canine-acute-pancreatitis/
- Plumb, D. (2018). Plumb's veterinary drug handbook / Donald C. Plumb, Pharm. D. (Ninth ed.).
- Mazzaferro, Elisa M. (2017). Blackwell's Five-Minute Veterinary Consult Clinical Companion (2nd ed.). Hoboken: John Wiley & Sons, Incorporated.