Gastric Dilatation and Volvulus: A Case of Deadly Rotation
Written by Bailey Decker • 2024 Scholar
History
Koda is a six year old, spayed female, German Shepherd mixed dog that was presented to IVS for continuous pacing, panting, non-productive retching, and an uncomfortable abdomen. Koda was transferred to IVS for surgical consultation following initial diagnostics and stabilizing care at another local emergency hospital.
Physical Exam Findings and Diagnostics
Upon physical examination, it was noted that Koda was panting and had significant distention of her abdomen, which was tympanic. Her abdomen was uncomfortable but soft during palpation. Koda’s mucus membranes were injected, but she had strong synchronous femoral pulses. Her temperature was mildly hypothermic at 98.3?. Koda’s other vital parameters were within normal limits. She was ambulatory, and neurologically appropriate. Her body condition score was 8/9. Koda was clinically stable, though uncomfortable.
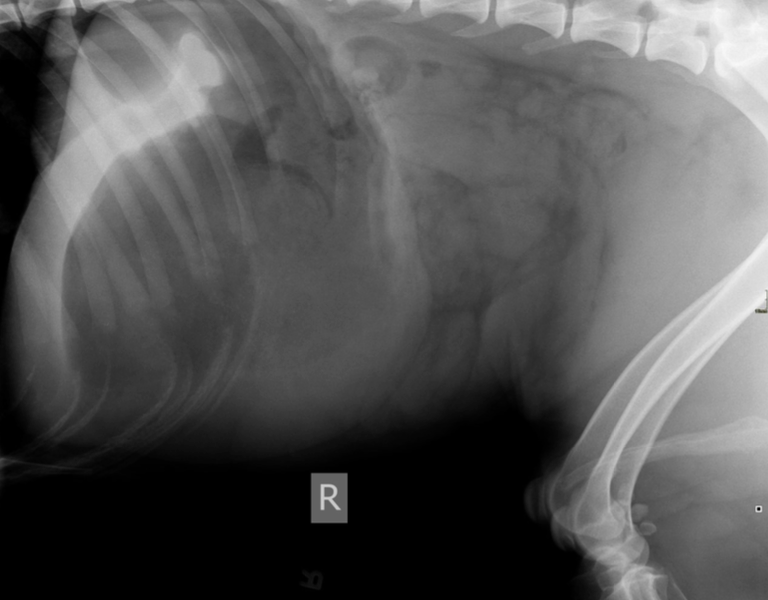
Radiographs, preferably a right lateral image were performed by the referring hospital. Koda’s images were interpreted by IVS’s Dr. Hoyt, and revealed a classic gas pattern referred to as “Popeye’s arm”. Bloodwork, including a complete
blood count, chemistry and electrolyte panel, lactate, and a PT/PTT all had values within the normal reference interval.
Diagnosis
A diagnosis of Gastric Dilatation and V olvulus (GDV), commonly called bloat by laymen, was confirmed by Dr. Hoyt.
What is Gastric Dilatation and Volvulus
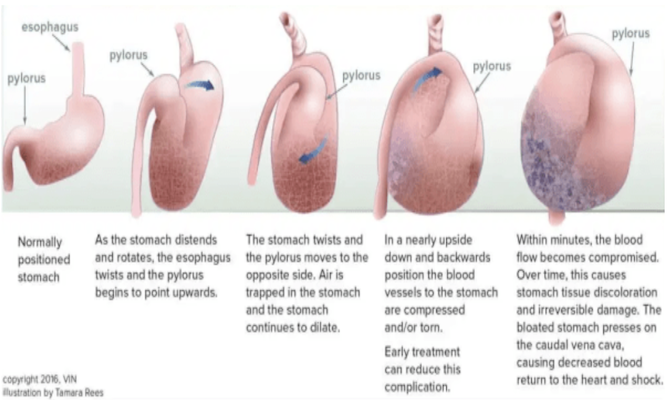
GDV is a true surgical emergency in which gastric distention and malpositioning, caused by rotation of the stomach around the mesenteric axis, creates extreme pain due to increased intragastric pressure and vascular compromise leading to circulatory shock. Deep chested breeds of dogs including Great Dane, German Shepherds, Labradors, and the Setters have genetic predisposition to the condition, though any breed may develop GDV . Other factors have also been linking to the development of GVD include a first degree family member who had GDV, underweight body condition, rapid ingestion of food/ aerophagia, small kibble size, eating only one meal per day, exercising vigorously after a meal, a fearful or aggressive temperament, and stressful events (temperature extreme, boarding, etc.). In commonly afflicted breeds, owners may elect for prophylactic gastropexy at the time of spaying or neutering to reduce the risk of GDV later in life.
Due to the canine anatomy, more invasive intervention like partial gastrectomy and splenectomy may also be necessary. Complications include gastric necrosis, hypoxemia of tissues, splenic entrapment, excessive internal bleeding, development of shock, cardiac arrhythmia, aspiration/ pneumonia, sepsis, and adverse anesthetic events may occur. Prognosis is considered guarded to grave depending on the patient's presentation, with studies indicating that even with ideal intervention mortality rates are commonly 10-20% with some studies citing up to 45%.
Common abnormal elevations on lab work for dogs suffering from GDV would include PCV , total solids, electrolytes, blood glucose, and lactate. Pre-renal azotemia, Creatinine Kinase, ALT, AST, and serum potassium elevations are not unusual findings secondary to systemic hypotension and hypoxic tissue damage. Hyperlactatemia (>6 mmol/L) is correlated with gastric necrosis, increasing the likelihood that a partial gastric resection is needed.
Treatment
Koda had arrived at IVS with a shaved area on her left abdomen from decompression gastric trocarization performed by the referring hospital service. Similarly, Koda also had an intravenous catheter in her cephalic vein and had received a 20mL/kg Fluid bolus (1000mL), 4mcg/kg of Fentanyl IV for pain, and cerenia at 1 mg/kg.
Her owners were informed of her diagnosis and the necessity of performing an abdominal exploratory surgery with derotation and gastropexy. A second IV catheter was placed in a rear saphenous vein and prepped for surgery. Koda received phylyte at 250mL/hr. Her anesthetic protocol included sedation with midazolam and dexmedetomidine, induction with propofol, and maintained on Isoflurane. She was monitored continuously via ECG, blood pressure readings,
and manual vital observations.
A midline incision was made, through which Dr. Hoyt visualized the stomach, it was hyperemic, but the tissue was viable. Decompression of the stomach was achieved with an orogastric tube. Then, the stomach was rotated counterclockwise to attain a correct position. The spleen and proximal GI tract were assessed for viability and bleeding. Once satisfied that no additional surgical intervention would be needed, Dr. Hoyt performed an incisional gastropexy,
affixing the gastric antrum to the abdominal wall over the last rib. The abdomen was then lavaged with a liter of warmed saline, suctioned, then closed.
Koda experienced some hypothermia, but recovered uneventfully from surgery. She was managed in hospital with a Fentanyl CRI, IV fluid therapy, and three doses of IV cefazolin. Food was withheld for 8 hours post operation. Koda recovered well, regained an appetite, and was able to transition to oral formulations of Gabapentin, Codeine, Trazodone, and Ondansetron. She was successfully discharged to her owners for ongoing care.
References & Citations
- Dr. D.J. Brockman, “Gastric Dilatation and V olvulus”, World Small Animal and Veterinary Association World Congress Proceedings 2008, Department of Small Animal Medicine & Surgery, Royal V eterinary College North Mymms, Hatfield, Herts, UK https://www.vin.com/apputil/content/defaultadv1.aspx?pId=11268&id=3866525
- Dr. Thomas W. G. Gibson, “Gastric Dilation and V olvulus in Small Animals (Bloat)” Merck Professional V eterinary Manual Online Edition. Jun. 2020.
https://www.merckvetmanual.com/digestive-system/diseases-of-the-stomach-and-intestines-in-small-animals/gastric-dilation-and-volvulus-in-small-animals - Image Courtesy of Dr. Thomas W. G. Gibson, “Gastric Dilation and V olvulus in Small Animals (Bloat)” Merck Professional Veterinary Manual Online Edition. Jun. 2020. https://www.merckvetmanual.com/digestive-system/diseases-of-the-stomach-and-intestines-in-small-animals/gastric-dilation-and-volvulus-in-small-animals
- Dr. Kari Rothrock, “Gastric Dilatation - V olvulus Syndrome” VinCyclopedia of Disease, Revised August 4, 2022. https://www.vin.com/members/cms/project/defaultadv1.aspx?pId=607&catId=143175&id=7208182&ind=289&objTypeID=1008