Nellie's Case Summary
Written by Lizeth Lopez, 1st year veterinary student • 2021 Scholar
History
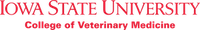
On July 5, 2021, Nellie, an 8-month-old female spayed miniature schnauzer, came into Iowa Veterinary Specialties (IVS) for a triage due to a partial evisceration (exposed intestines and omentum (see figure 1)). The owner stated Nellie was spayed 5 days prior and was running around in the backyard 30 minutes before bringing her into IVS.

Figure 1: Spay site dehiscence with intestinal evisceration. Nellie’s blue and black surgical shirt prevented complete contamination of the exposed intestines and omentum.
Physical Exam
Upon the initial examination, Dr. Braas discovered a spay site dehiscence; a portion of Nellie’s intestine was contained within the omentum and exposed to the environment. Dehiscence is an incisional hernia caused by disruption of wound edges. Excessive forces placed on the incision like intrabdominal pressure, muscle tension or uncontrolled activity can cause abdominal wall dehiscence. Dehiscence most commonly occurs within 3 to 5 days postoperatively.
On presentation, minimal contamination was visible as the small intestine and omentum were contained within the surgical shirt (see figure 1). Nellie weighed 18.8 pounds, was panting, had pale mucous membranes, a temperature of 101.8F (normal= 100-102.5F), heart rate of 80 beats per minute (dog normal= 60-160 bpm), and a pain score 3 out of 4.
Diagnostics
A complete blood count (CBC) and chemistry panel were performed prior to medicating or sedating Nellie to determine if organs were functioning properly, to evaluate electrolytes, and to check for infection or secondary septic peritonitis (inflammation of the abdominal cavity membrane lining due to infection). Secondary septic peritonitis can be life threatening because it can cause decreased circulatory volume due to the excessive loss of proteins, electrolytes and fluid in the abdominal cavity. The decreased circulatory volume can result in hypovolemic shock, which can lead to tissue hypoxia causing organ failure and eventually death if left untreated.
Signs of sepsis or septic peritonitis:
- Low glucose levels can indicate signs of sepsis because bacteria use glucose as an energy source.
- Elevated lactate levels can indicate signs of sepsis. Lactate is an indicator of decreased organ perfusion, decreased oxygen delivery or extraction.
- Decreased heart rate or bradycardia can occur in late shock (increased heart rate or tachycardia can occur in early shock).
- Low blood pressure due to decreased circulatory volume.
- Elevated levels of neutrophils as the body tries to fight off infection.
CBC results: patient’s blood cells are evaluated:
- Leukopenia (3.75K/uL): decreased number of white blood cells
- Neutropenia (1.72K/uL): abnormally low numbers of neutrophils in blood, can lead to increased infection susceptibility
- high mean platelet volume (MPV) 14.8fL: used to measure the average size of platelets
Chemistry panel results: measures organ function and electrolyte balance
- low amylase (346 U/L): no clinical significance
- hypokalemia (low potassium 3.2mmol/L): could be due to dehydration or kidney failure, can cause a decrease in heart rate
Stabilization Plan
Placed an intravenous catheter to administer an intravenous fluid bolus of 150ml isotonic solution to increase cardiac output, restore organ blood flow and improve blood pressure. Performed an emergency surgery to repair the spay site dehiscence. Decreased pain by administering hydromorphone.
Surgery
After inducing anesthesia with alfaxalone, Nellie was intubated and maintained on isoflurane for the duration of the procedure. The affected area was clipped and prepped for surgery (shown in figure 2).

Figure 2: Katie (Surgery Technician) clipped the surgical area before prepping for surgery.
The omentum covering the intestine was examined and a portion that had been exposed was properly clamped, ligated and removed. Further examination was conducted to determine if there was a need for intestine resection, fortunately, the remaining intestines were pink, which meant proper perfusion (adequate blood flow) and peristalsis. Although the mesentery had some bruising, no bleeding was observed. The uterine ligature remained intact and secure (see figure 3).

Figure 3 to the left: Dr. Braas evaluating the intestine as she rinsed it with 60ml of warm saline in a 60cc syringe with an 18G catheter. Saline soaked lap sponges surrounded the intestine to protect it from drying.
With no observed hemorrhage, the abdomen was lavaged with 1L of warm saline (shown in figure 4).

Figure 4: Abdomen was lavaged copiously by Dr. Braas with 1L of warm saline.
The skin edges, subcutaneous tissue, and body wall were debrided and freshened prior to closing each layer (see figure 5 and 6).
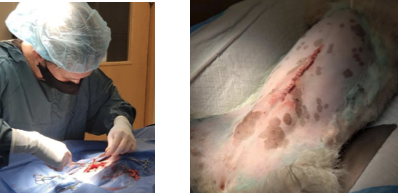
Figure 5 (left): Dr. Braas debriding the skin edges. Figure 6 (right): Nellie’s skin closed with staples.
Medications
Medication overnight at IVS:
- Intravenous Ampicillin Sulbactam (Unasyn): injectable antibiotic (beta-lactamase inhibitor) used to prevent infection
- Intravenous Enrofloxacin (Baytril): antibiotic (fluoroquinolone carboxylic acid derivative) used to treat bacterial infections
- Intravenous Isotonic electrolytes: maintains perfusion
- Fentanyl-Lidocaine-Ketamine constant rate infusions (FLK CRI): used to manage pain
Medication to go home:
- Amoxicillin/clavulanate: antibiotic (beta-lactamase inhibitor) used to treat bacterial infections
- Enrofloxacin: antibiotic used to treat bacterial infections
- Meloxicam: a non-steroidal anti-inflammatory drug that also serves as pain medication
Prognosis
Prognosis for Nellie was fair. No hemorrhage or leakage was observed during surgery and the intestines were viable. A recheck in 12 days was scheduled for Nellie’s suture removal. Owner was instructed to limit physical activity that could compromise or delay the recovery time.
Negative prognostic indicators: localized infection, sepsis, hemorrhage, necrosis (death of cells in an organ or tissue), peritonitis (inflammation of the abdominal cavity wall), or surgical site dehiscence.

Figure 7: Nellie recovering from surgery with an E-collar to prevent unwanted licking at the surgery site.
References & Citations
- “Emergency Management of Specific Conditions.” Kirk and Bistners Handbook of Veterinary Procedures and Emergency Treatment, by Robert Warren Kirk et al., Elsevier, 2012, pp. 77–83.
- “Peritonitis.” Emergency Procedures for the Small Animal Veterinarian, by Signe J. Plunkett, Saunders Elsevier, 2013, pp. 255–264.
- Ragetly, Guillaume R, et al. “Septic Peritonitis: Treatment and Prognosis.” VetFolio, 8 Mar. 2019, www.vetfolio.com/learn/article/septic-peritonitis-treatment-and-prognosis.
- “Septic Peritonitis.” Blackwell's Five-Minute Veterinary CONSULT Clinical Companion, by Elisa M. Mazzaferro, WILEY Blackwell, 2018, pp. 672–681.